Despite what your mother told you, time cannot mend all broken hearts, but current research indicates that cord blood and cord tissue stem cells may be able to help heal the real thing.
Heart disease literally hardens the heart
Heart disease is the number one cause of death for both men and women in the United States. Because the cells of the heart do not replace themselves naturally, those who have suffered from heart disease may have few treatment options available.
Heart Disease
Heart disease is an umbrella term for many kinds of heart conditions. Coronary heart disease, also called coronary artery disease, is the most common and also the source of most heart attacks. A heart attack happens when the organ is starved of oxygen, such as when a clot blocks the flow of blood. A heart attack will leave behind scar tissue that lacks muscle or blood vessels. Any part of the heart, which is basically a big muscle, that can’t contract, doesn't have a sufficient blood supply or otherwise limits the ability to pump blood could lead to further complications.
Take Heart with Stem Cells
Stem cells offer hope in the fight against heart disease. Stem cells may be used to help replace the damaged heart tissue and valves and establish new vessels to supply them with blood. Stem cells could also be used to build new heart tissue, even whole new hearts. The American Heart Association (AHA) estimates that 84 million people who currently suffer from cardiovascular disease might one day be cured or treated through stem cell breakthroughs.
Scientists have their hearts set on it
About a decade and a half ago, scientists began testing the effectiveness of stem cells in regenerating heart tissue by simulating heart attacks in mice and rats and then repairing the damage with heart cells grown from stem cells. In 2001, scientists reported that after they injected stem cells into the damaged wall of the ventricle, these cells led to the formation of new cells, which in turn developed into coronary arteries, arterioles and capillaries. The newly formed arteries, arterioles and capillaries occupied 68 percent of the damaged portion of the ventricle nine days after the stem cells were transplanted, in effect replacing the dead tissue with living, functioning tissue. The researchers found that mice that received the transplanted cells survived in greater numbers than mice with heart attacks that did not receive the mouse stem cells.
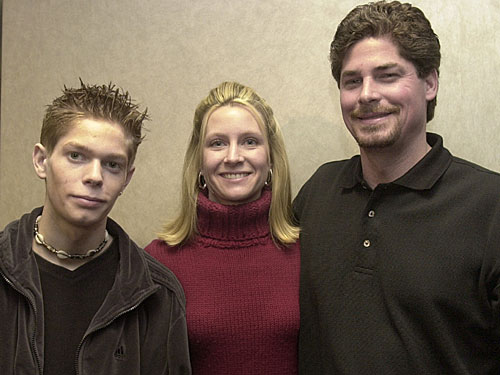
Dimitri Bonnville (left), with the approval of his parents (right), was the first human to receive an experimental stem cell therapy to repair his heart
(Via Wired)
In 2003, sixteen-year-old Dimitri Bonnville became the first human to receive experimental stem cell therapy to revive his damaged heart tissue. Bonnville had been accidentally shot in the heart with a nail gun while doing home repair. He underwent open-heart surgery but later suffered from a massive heart attack. In lieu of heart transplant surgery, Bonnville’s parents opted for a stem cell therapy to repair his damaged heart. Doctors at the William Beaumont Hospital in Michigan harvested his stem cells, and using a heart catheter, they transplanted the stem cells into the artery that supplies blood to the front of the heart. Following the procedure, Bonnville experienced significant improvement in heart function.
In 2004, the FDA approved the first clinical trial in the United States to test stem cell therapy for severe heart failure. Prior to this clinical trial, scientists in Brazil had already tested the treatment on fourteen patients. The 2014 study's results, published in Circulation Research, showed that the procedure is safe and significantly improves heart function.
“We saw significant improvements in exercise capacity,” said Emerson Perin at the Texas Heart Institute in Houston, Texas. “This is measured in terms of peak oxygen capacity, which went from 17 percent to 24 percent in treated patients.”
Further studies followed such as the one highlighted in a 2007 article in the International Journal of Cardiology. It reported on a study that divided 70 cardiac patients into two equal groups: one group was injected with stem cells, and the other group received a placebo. Six months later, the patients treated with stem cells had a significant improvement in left ventricular pumping, and in the control group, there was no improvement. Twenty-five patients experienced complications, but none died.
Following these studies, from 2009 to 2011, a number of statin drugs, which are used to treat high cholesterol, showed that they could enhance the efficacy of stem cells in cardiac repair.
“The finding that a drug with an excellent safety profile used widely to lower blood cholesterol is effective in improving cardiac function in hibernating myocardium is a welcome finding,” said Gen Suzuki, M.D., Ph.D., UB research assistant professor of medicine and the author of a study on one such drug.
Statin drugs showed promise, but attention on their abilities to improve outcomes has waned in recent years.
HLHS in Newborns
A study looking at safety and feasibility of infusing cord blood stem cells into the hearts of babies born with a defect known as hypoplastic left heart syndrome (HLHS) is nearing completion, and we have already heard of one family who is sleeping better knowing their little boy is on the road to recovery.

Rylas Sexton was 1 of 5 children to participate in the clinical trial
HLHS occurs in approximately 1,000 births each year in the United States and is when the left side of the heart does not fully develop. The child must undergo a series of three surgeries over the same number of years to effectively re-plumb the blood flow to the heart.
“Prior to the 1980s and '90s, there were essentially no good surgical options for these patients,” said Dr. Joe Rossano, who heads up the cardiac center at the Children's Hospital of Philadelphia, “but a number of very innovative surgical techniques were developed that have allowed many of these children to survive and thrive." Children's Hospital of Philadelphia, known as CHOP, is one of the leading medical centers for HLHS surgeries and treatment.
The surgeries allow the children to live relatively normal lives, but because the right side of the heart is handling the tasks of both ventricles, it has been shown to weaken with age. This would normally require the patient to undergo a heart transplant later down the road, but researchers think an infusion of cord blood could solve the problem by making the right side of the heart two times to five times stronger.
“We're finding ways of inventing new therapies to make that right heart stronger by stimulating the growth of the heart muscle and make the five-horsepower engine, a 10-horsepower engine, a 50-horsepower engine,” said Dr. Tim Nelson, who researches and conducts new HLHS treatments. “And if we make it strong enough, we believe that that has a shot at delaying and preventing transplant for a significant number of these children."
Andrea and Heath Sexton found out their son Ryals would be born with HLHS during one of their routine ultrasounds.
"We were wondering how is this going to change our lives ... Obviously, the care of a child that possibly would need a lot of help, maybe a lot of long-term help," said Heath Sexton. "And then, of course, in the back of your mind, obviously, you've read that a lot of children don't make it past three months. And, so, just thinking about, you know, am I going to be prepared ... for a funeral?"
CHOP became one of a number of institutions who joined together to help expand access to this clinical trial, and the Sextons quickly put their child in the care of the CHOP as the first family to undergo the treatment. After collecting the cord blood at the time of birth, processing it in Minnesota and cryo-preserving it for three months, the cord blood stem cells were thawed and infused directly into Ryals’s heart near the end of his second operation. In three more years, Ryals will undergo the final surgery. His family is just happy to have him home in Alabama and feel much better now that they are able to give some normalcy to Ryal’s life—and future.
Building one's heart's content
In addition to being able to repair heart damage through the transplantation of stem cells into the affected area, doctors have been able to grow heart parts in the lab to eventually be placed in a damaged heart. In 2007, Sir Magdi Yacoub, a world-famous heart surgeon based at Imperial College London, and a team of researchers developed heart valve cells with stem cells. They used collagen to hold the valve tissue in shape as it grew into one-inch disk-shaped valves. Although plastic heart valves do exist, stem cell–grown valves offer a distinct advantage: "[B]ecause the patient's own stem cells are used, it eliminates the problem with rejection that happens when a heart has been donated by another person."
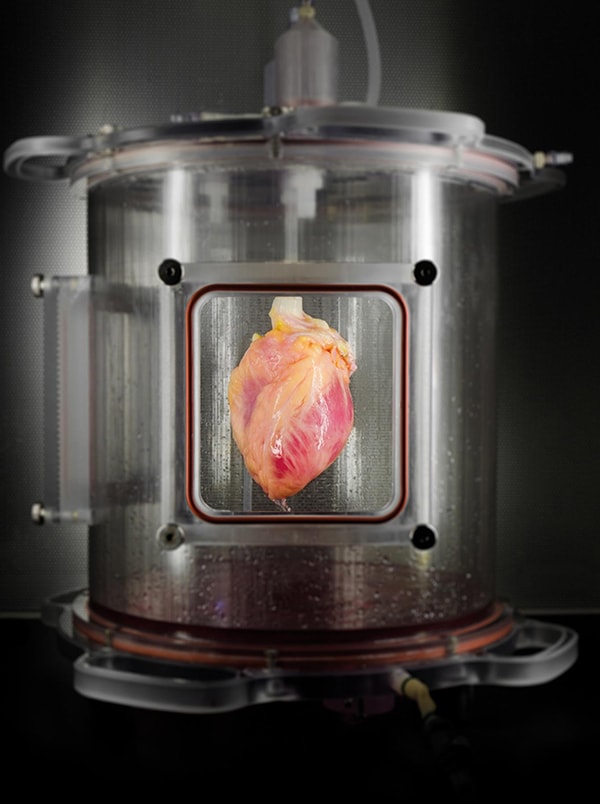
Full-sized human heart grown from stem cells
Presenting at the American Heart Association's annual scientific sessions in New Orleans during November 2008, cardiac surgeon Dr. Ralf Sodian reported that his team had used stem cells derived from umbilical cord blood to create tissue-engineered heart valves. Stem cells collected at birth from the umbilical cord may help doctors fashion new heart valves for children born with heart valve defects. The tissue-engineered valves would have the advantage of growing with the child, said researchers at the University Hospital of Munich.
"If we replace a valve in a child, they will need surgery several times in their lifetime because they will grow out of the devices, so the ultimate goal is to have a construct which is able to grow with the child and only have to do the surgery once," said Dr. Sodian.
In addition, stem cell-based valves offer the advantage of not experiencing the wear-and-tear issues related to metal and plastic valves.
In February 2009, researchers at the University of Wisconsin–Madison announced that they had taken skin cells and grown them into pulsing heart cells. In Circulation Research, Timothy Kamp, co-director of the university's Stem Cell & Regenerative Medicine Center, reported that the reprogrammed heart cells made in the laboratory generated electrical pulses, and in response to these pulses, they contracted. It is the collective contraction of all these cells that enables the heart to beat.
"It's an encouraging result because it shows that those cells will be useful for research and may someday be useful in therapy,'' said Kamp. "If you have a heart failure patient who is in dire straits and there are never enough donor hearts for transplantation, we may be able to make heart cells from the patient's skin cells and use them to repair heart muscle. That's pretty exciting."
More recently with the advent of 3-D printing, scientists are working toward a future where body parts bioengineered from stem cells will be able to engrafted into the human body.
Getting to the heart of the matter
A 2014 meta-analysis of 23 randomized controlled trials involving 1,255 participants showed a reduce risk of mortality or re-hospitalization in the long-term for patients who underwent a stem cell therapy for heart disease. Unfortunately, despite some promising results, the diverse content and character of these studies and the limited understanding of basic principles, pathways and other factors have slowed progress, especially as it has to do with the one of the most complex muscles in the human body.
As scientists have been better developing an understanding of how these stem cells are aiding heart repair, they have moved more and more towards mesenchymal stem cells as a source. While found in cord blood, mesenchymal stem cells can be found in greater abundance in cord tissue. Studies using other sources of these mesenchymal stem cells such as bone marrow will continue to be performed, but cord tissue–derived mesenchymal stem cells have shown to have a higher proliferative potential and to be capable of differentiating into more cell types. Unfortunately, as the stem cells in cord tissue have only recently been discovered, their availability—especially in self-treatments—is greatly limited.
Between 2010 and 2015, there have been about 41 clinical trials performed using mesenchymal stem cells (MSCs) in cardiac repair. Most of these studies were in the processing of completing phase II and some were even moving into phase III. Today, more and more clinical trials using stem cells like those found in cord tissue are being used to treat heart disease. One of the larger such studies was completed in 2016. The phase II study showed significant improvements in the long-term health of the 58 patients with class III or class IV heart failure who received their own stem cells.
As scientists gain further insight into how, when, which and to what capacity stem cells can be used to treat heart conditions through these clinical trials, we grow ever closer to potentially discovering a whole new way to mend a broken heart.
Current Clinical Trials
The phase I trial using cord blood to treat HLHS is still recruiting with a number of collaborating hospitals.
A similar clinical trial is being conducted out of the Royal Children's Hospital in Australia.
A pair of clinical trials in China and a clinical trial in Turkey are similarly using cord tissue to treat chronic ischemic cardiomyopathy.